Understanding Endoscopic Rhizotomy
An endoscopic rhizotomy is a minimally invasive procedure designed to target small nerve branches that transmit pain signals from the spine. By treating these nerves directly, the procedure helps reduce chronic back pain, muscle spasms, and discomfort during certain movements. Because the technique uses a tiny incision and specialized imaging, it preserves surrounding tissues and allows for a faster recovery. Many patients experience meaningful relief while maintaining normal spinal mobility.
How the Procedure Works
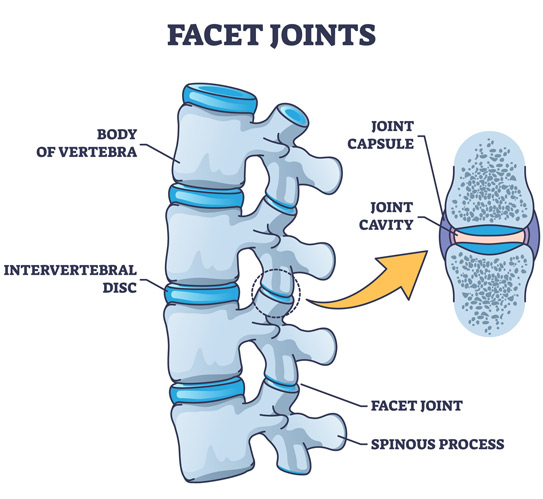
During an endoscopic rhizotomy, a surgeon uses a small incision to access the medial branch nerves that carry pain signals from the facet joints. A narrow tube is inserted near the affected area, followed by a high-definition camera that provides a clear internal view. Using precise instruments, the surgeon ablates the targeted nerve to interrupt the pain pathway. This focused approach allows for effective treatment without disturbing nearby muscles or structures.
The procedure is commonly used for patients with facet joint–related pain, including facet arthritis, chronic low back pain, and persistent symptoms following previous spine treatments. Individuals who have responded temporarily to medial branch blocks or percutaneous rhizotomy often benefit from this technique. By targeting specific nerve branches, endoscopic rhizotomy aims to provide longer-lasting relief.
Preparing and Knowing What to Expect
Before the procedure, patients are typically instructed to avoid eating or drinking and to arrange transportation home. Physicians may review current medications and advise which ones should be paused. During the procedure, patients lie on their stomach while a nurse places an IV line and administers local anesthesia. A small tube is inserted near the facet joint so the surgeon can visualize and treat the medial branch nerve.
Patients may feel pressure but should not experience pain during the procedure. Treatment generally takes 30 to 60 minutes, followed by brief monitoring before discharge. Recovery is usually quick, and most individuals return to regular activities the next day while avoiding strenuous exertion. Mild soreness or bruising at the incision site may occur and can be eased with ice or over-the-counter medication.

Eligibility and Candidacy
Candidates for endoscopic rhizotomy are typically individuals with chronic back pain linked to facet joint dysfunction. Patients who experienced temporary relief from a medial branch block or percutaneous rhizotomy may be good candidates for the endoscopic approach. Those with persistent symptoms lasting more than six weeks or who notice increased spasms with pressure on the lower back may also benefit. A thorough evaluation helps determine whether this treatment is appropriate.
Aftercare and Potential Risks
Following the procedure, patients can often resume normal routines within a day, although heavy lifting and vigorous exercise should be avoided initially. Showering is permitted, but soaking in baths, pools, or hot tubs should be postponed for 24 hours. Common side effects include temporary soreness, swelling, or mild bruising at the incision site.
While complications are uncommon, patients should contact their physician if they experience persistent numbness, dizziness, weakness, fever, chills, nausea, or worsening redness or drainage at the incision site. Monitoring symptoms and following post-procedure instructions support safe healing and long-term comfort.